In spondylolisthesis, one of the bones in of the spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar spine). In some people, this causes no symptoms at all. Others may have back and leg pain that ranges from mild to severe.
Many types of spondylolisthesis can affect adults. The two most common types are degenerative and spondylolytic. There are other less common types of spondylolisthesis, such as slippage caused by a recent, severe fracture or a tumor.
Due to the aging process, general wear and tear causes changes in the spine. Intervertebral disks begin to dry out and weaken. They lose height, become stiff, and begin to bulge. This disk degeneration is the start to both arthritis and degenerative spondylolisthesis (DS). As arthritis develops, it weakens the joints and ligaments that hold the vertebrae in the proper position. The ligament along the back of your spine (ligamentum flavum) may begin to buckle. One of the vertebrae on either side of a worn, flattened disk can loosen and move forward over the vertebra below it. This slippage can narrow the spinal canal and put pressure on the spinal cord (spinal stenosis). Women are more likely than men to have DS, and it is more common in patients who are older than 50. A higher incidence has been noted in the African-American population.
One of the bones in the lower back can break and this can cause a vertebra to slip forward. The break most often occurs in the area of your lumbar spine called the pars interarticularis. In most cases of spondylolytic spondylolisthesis, the pars fracture occurs during adolescence and goes unnoticed until adulthood. The normal disk degeneration that occurs in adulthood can then stress the pars fracture and cause the vertebra to slip forward. This type of spondylolisthesis is most often seen in middle-aged men. The back pain is sometimes accompanied by leg pain.
“Most patients with this condition do not experience pain and may be surprised to find they have a slippage when it comes up in x-rays,” explains Dr. Athanassious. Although nonsurgical treatments will not repair the slippage, many patients report positive results from therapy and exercise. Surgery may be recommended after 3-6 months of failed improvement and patients may be unable to walk or stand, and experience debilitating pain and weakness.
Surgery for both conditions includes removing the pressure from the nerves and spinal fusion. This involves opening up the spinal canal in a procedure called a laminectomy. Spinal fusion is essentially a “welding” process. “This technique is used to fuse together the painful vertebrae so that they heal into a single, solid bone,” says Dr. Athanassious. Fusion surgery recovery takes several months while comfort levels improve much more quickly.
About Dr. Athanassious and SRO

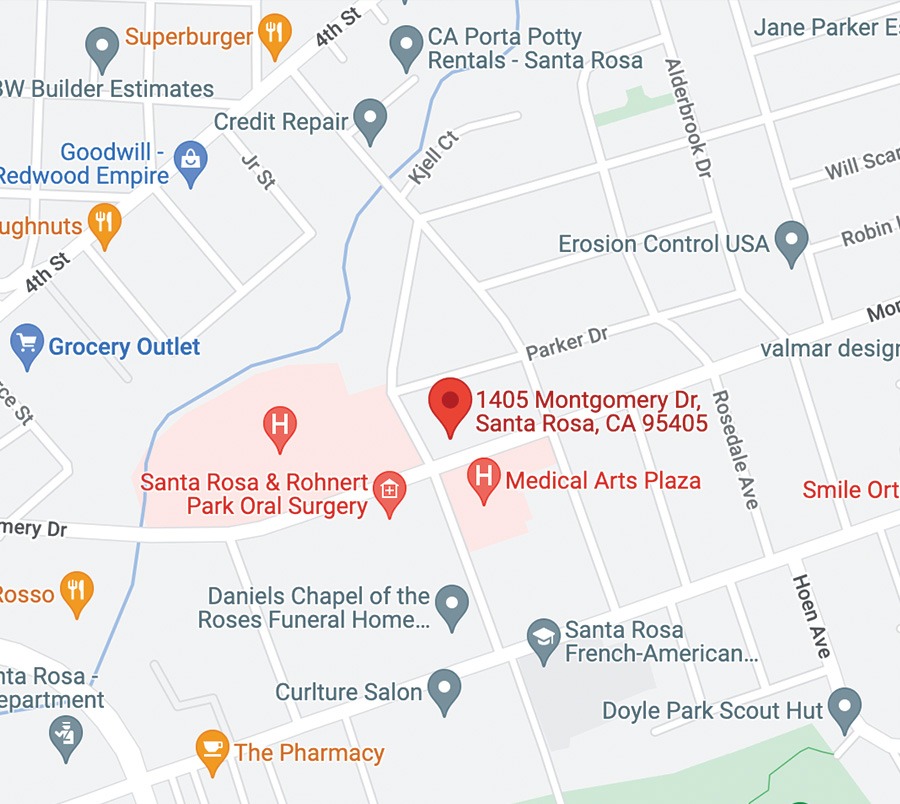
The Total Spine Health Program at Santa Rosa Orthopaedics strives to do everything possible to get patients back to doing the things they love most. When surgery is necessary, Dr. Athanassious carries fellowship training in the most advanced spinal surgery and injection procedures from the prestigious Stanford University. For more information about SRO surgeons and services, visit srortho.com.
For more information on spinal fusion visit The Total Spine Health Program or call 707-546-1922.