Knee joint injuries are typically related to sports, such as football, rugby or ice hockey, but people often do not know that such injuries may lead to joint inflammation and post-traumatic osteoarthritis. In advanced post-traumatic osteoarthritis, joint cartilage breaks down completely, causing severe joint pain, lack of mobility and even social isolation. However, the mechanisms leading to osteoarthritis are not known. Currently, it is not possible for a physician examining a patient to predict future joint condition and possible development of osteoarthritis. In the future, however, this may be possible, as a new study from the University of Eastern Finland and Massachusetts Institute of Technology now shows that articular cartilage degenerates specifically around injury areas when the fluid flow velocity becomes excessive. The findings were reported in Scientific Reports.
The study presents a new mechanobiological model for cartilage degeneration by implementing tissue deformation and fluid flow as mechanisms for cartilage breakdown when a normal dynamic loading, such as walking, is applied to the joint. The results were compared to experimentally observed degradation of articular cartilage. Ultimately, the new model could be used to predict osteoarthritis in personal medicine, to suggest optimal rehabilitation protocols, and to improve the quality of life.
The researchers found that different mechanisms, such as fluid flow and tissue deformation, can cause cartilage degradation after a knee injury. The results obtained using the novel algorithm agreed well with the experimentally observed proteoglycan content and cell death in cartilage samples. According to the researchers, a numerical analysis shows that both fluid flow and tissue deformation are plausible mechanisms leading to osteoarthritis, but increased fluid flow from cartilage seems to be better in line with the experiments.
“Our findings indicate that after an injury in the knee and subsequent tissue loading, osteoarthritis is caused by easy leakage of proteoglycans through the injury surface by high fluid outflow,” Early Stage Researcher Gustavo A. Orozco from the University of Eastern Finland explains.
The findings are significant, and could open up new avenues for the model to be employed in the prediction of subject-specific progression of post-traumatic osteoarthritis, and in the evaluation of the effect of clinical interventions in the future. Specifically, the model could identify high and low-risk lesions in the cartilage for osteoarthritis development and suggest an optimal and individual rehabilitation protocol.
Treating Osteoarthritis of the Knee
Many knee injuries including osteoarthritis can be successfully treated with a change in lifestyle, using braces to support the joint, injections to relieve pain and rehabilitation exercises. Other injuries may require surgery to correct. An injured knee can obviously affect mobility, and clearly a healthy knee is necessary for basic every day movements such as sitting, standing and walking. But chronic, unrelenting knee pain can also lead to health complications and certainly diminished quality of life. When all else fails, Total Joint Replacement (TJR) is one option that proves beneficial in many cases.
What is TJR
Total joint replacement is one of the most successful contemporary surgical procedures thanks to refined surgical techniques, improved implant characteristics, aggressive physical rehabilitation and a focus on pain management, all of which have contributed to the success of TJR. Total joint replacement surgery, also known as arthroplasty, works to repair severe injuries or to replace joints destroyed by arthritis and other bone diseases. It is performed to replace the ends of both bones in a damaged joint to create new joint surfaces. Weight-bearing joints are naturally under the greatest strain and are more likely to lose protective cartilage over time, particularly in the hips and knees.
Santa Rosa Orthopaedics also offers a revolutionary surgical option for some joint replacement patients using the robotic assisted device called RIO Robotic Arm Interactive Orthopedic System. This highly advanced procedure is essentially a minimally invasive technique that reduces damage to the bone and surrounding tissue for faster recovery. The MAKO® system is currently available primarily for partial knee replacement and is offered by both Dr. Michael McDermott and SRO’s Dr. Nathan Ehmer at Sutter Santa Rosa Regional Hospital.
About Santa Rosa Orthopaedics
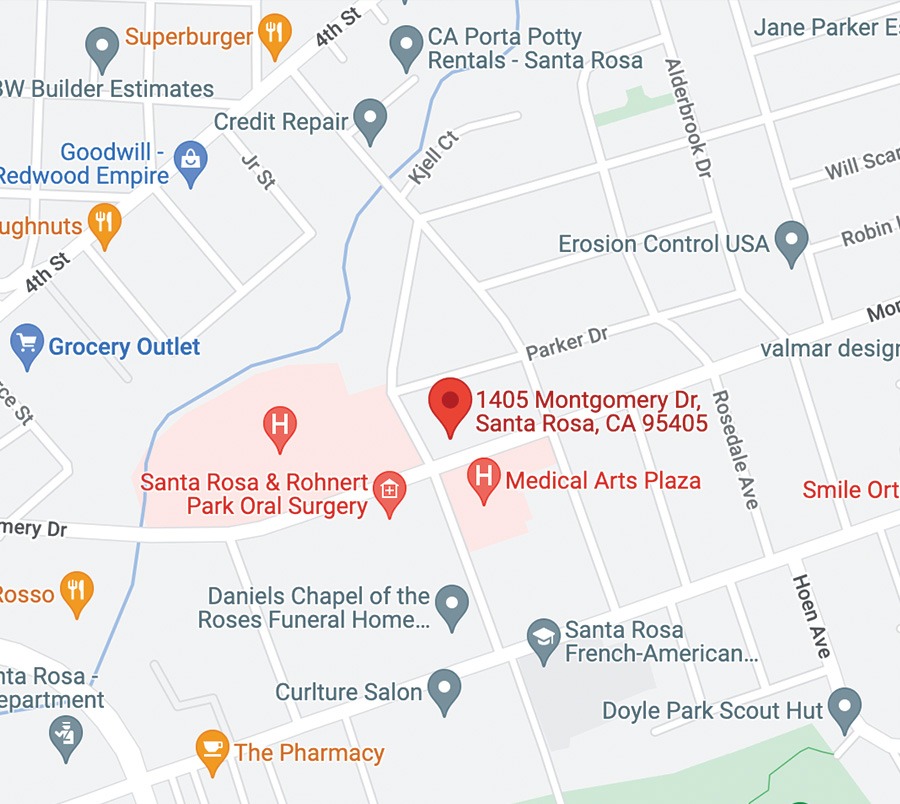
At Santa Rosa Orthopaedics (SRO), a collaborative team of multi-specialist orthopedic surgeons and experienced physical and occupational therapists work together to bring the best outcomes to patients dealing with chronic knee issues including pain relief, recovery and rehabilitation.
SRO has set the model for exceptional orthopedic care for more than 60 years. In addition, SRO offers a broad range of nonsurgical and surgical treatments aimed at conditions that commonly affect bones, joints, tendons connective tissues and ligaments. To make an appointment or to learn more about SRO Orthopedic Surgeons, please visit the SRO website.
Story Source — Read this article on Science Daily – University of Eastern Finland. “Why knee joint injury leads to osteoarthritis.” ScienceDaily. ScienceDaily, 25 October 2018. www.sciencedaily.com/releases/2018/10/181025103315.htm.