Low-risk patients undergoing a total hip replacement with a posterior approach can skip the standard hip precautions currently recommended for post-surgical recovery, according to a new study conducted at Hospital for Special Surgery (HSS), in New York City. Eliminating standard precautions in this population did not increase the risk of hip dislocation, according to the research presented at the annual meeting of the American Academy of Orthopaedic Surgeons, March 12-16 (abstract #140).
“The majority of patients we see are low risk; 90% of patients probably qualify for minimized precautions,” said Peter Sculco, MD, the study’s lead author and an orthopedic surgeon specializing in hip and knee replacement at HSS.
In the last ten years, surgeons have started favoring the anterior approach (through the back of the hip) for total hip replacement over the posterior approach, because it doesn’t involve standard hip precautions. Little data, however, backs the standard hip precautions recommended for the posterior approach. For a posterior approach, standard precautions are not flexing your hip past 90 degrees, not internally rotating your hip more than 10 degrees, using an elevated seat cushion at all times and a grabber for anything that is on the ground, and sleeping on your back for six weeks.
“The precautions can be limiting and cause fear in patients,” said Dr. Sculco. “Sleeping on your back is very uncomfortable for many people. You often hear from physical therapists that patients are relieved when they can finally cross their legs and sleep on their side.”
The literature showing that hip precautions make a difference in hip dislocation is poor. “The current precautions are based on hip replacements done 25 years ago, and we have changed a lot in terms of improving how we do hip replacements that has given us more confidence in the stability of our hips,” said Dr. Sculco. “Our understanding of the dynamic movement of the pelvis and how we put the parts in is much different. The quality of our soft tissue repair and closure at the end of surgery is much more robust.”
When patients are on stringent precautions, they are not as active, which can hamper recovery. “If you minimize the hip precautions in an appropriate way, patients focus more on their mobility and recovery and less on the fear of how they turn their leg ten degrees,” said Dr. Sculco.
In the new study, researchers retrospectively reviewed all patients undergoing a posterior primary uncemented total hip replacement (total hip arthroplasty) from January 2014 to June 2016 at HSS. Surgeons had the choice to put patients on standard precautions or a pose avoidance protocol, to avoid a single pose, a flexed external rotation position that occurs when a person puts on their shoe or shaves their leg. A total of 1,311 patients met the inclusion criteria for the pose avoidance cohort, and the minimum followup was six weeks. Researchers then matched patients 1:1 in this group to a historical cohort of patients based on age, gender, and body mass index that were treated with standard posterior hip precautions.
Within the first six postoperative weeks, six dislocations occurred in the pose avoidance group (0.46%) compared with seven in the matched group (0.53%), a difference that was not statistically or clinically significant. “Our results suggest that the standard postoperative precautions in patients undergoing total hip arthroplasty through the posterior approach without known risk factors for instability are unnecessary,” said Dr. Sculco. “We may find that precautions don’t make sense for any of our patients, but we need to look at in a stepwise fashion.” Risk factors include neuromuscular issues, such as stroke, Parkinson’s disease and lumbar spine fusions.
The study was limited in that it is not a randomized controlled trial, usually the gold standard for dictating a change in practice. “The bottom line of the study is in recent years, we have learned more about interventions that matter after joint replacement and those that don’t really have efficacy. In most patients, we got rid of powerful anticoagulants, for example, and we are moving toward a shorter stay and even outpatient arthroplasty for total hip replacement,” said Dr. Sculco. “Minimizing precautions and simplifying the postoperative recovery is part of the larger simplification of surgery where we are using more selected resources and interventions for people, instead of blanketing everyone with the same kind of protocols.”
Dr. Sculco noted that there is an increasing demand for hip replacement in the United States. “In 2010, there were 310,000 hip replacements in the United States and that number is increasing. Its probably 350,000 if not more now,” said Dr. Sculco.
Story Source – Read this article on Science Daily: Hospital for Special Surgery. “Hip replacement patients can skip hip precautions, study suggests.” ScienceDaily. ScienceDaily, 12 March 2019. www.sciencedaily.com/releases/2019/03/190312170818.htm.
When to Seek Help for Hip Pain
When a patient has arthritis of the hip, the underlying bone can develop spurs and and other complications leading to pain and loss of motion. Total hip replacement can relieve pain and restore normal function in patients whose hip joint has been destroyed by trauma or disease. With total hip replacement surgery, the damaged hip socket and ball of the femur are replaced by implants. This type of surgery has been done successfully for more than years. Patients can expect the average hip replacement to last 20-30 years or more.
If a hip injury impairs a person’s ability to stand, bear weight and walk, consulting with an orthopaedic physician is the best bet. When pain is more gradual and does not respond to rest, ice and over-the-counter pain medications then seeking medical help is also a good idea. This is especially true if the hip pain begins to limit the range of motion of the hip or causes limping. Get medical help right away if:
- The hip pain came on suddenly
- A fall or other injury triggered the hip pain
- The joint looks deformed or is bleeding
- A popping noise in the joint when injury occurred
- Intense pain
- Inability to put weight on the hip
- Inability to move leg or hip
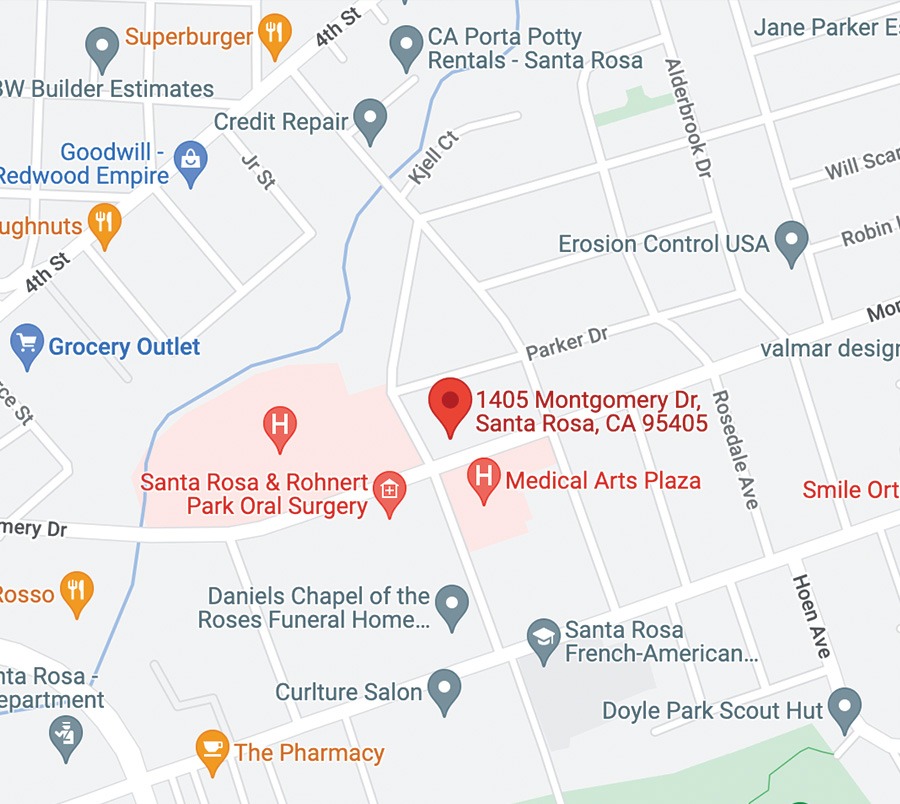
SRO Hip Replacement Specialists include Dr. Gary Stein, Dr. Nathan Ehmer and Dr. Michael McDermott. For more visit about total hip replacement visit our Total Joint Replacement section or call 707-546-1922.