Regenerative medicine is one of the most promising non-invasive technologies to come on the scene in the field of orthopaedics in some time. While surgical techniques in orthopaedics continue to advance for patients needing radical treatment for bone and joint issues, regenerative medicine provides a unique group of therapies that make it possible for physicians to support a patient’s own tissue regeneration. This technique can lead to long-term healing of what may otherwise be irreparable orthopaedic injuries.
Mesenchymal Stem Cells
Stem cell injection therapy utilizes something called mesenchymal stem cells (MSCs). These stem cells have the ability to become specialized types of cells, such as osteoblasts (bone cells), chondrocytes (cartilage cells), myocytes (muscle cells), and fibroblasts (ligament and tendon cells). MSCs can come from the umbilical cord blood of healthy donors under highly regulated circumstances, and they can be obtained from the patient’s bone marrow and/or adipose (fat) cells.
MSC treatment is considered a good option for treating musculoskeletal conditions involving lost or injured tissue, such as bone-on-bone arthritis; injury and tears to tendons, ligaments, and cartilage and degenerative disc disease. MSCs not only facilitate regeneration in various cell types within a joint, they also control the local inflammatory response.
Platelet Rich Plasma
Platelet Rich Plasma (PRP) Injections is a procedure that utilizes the patient’s own blood to form a concentration of blood cells called platelets. Platelets are among the many blood cells in plasma that not only play an important role in forming blood clots, but also contain growth factors that are central to the body’s healing process. When injected into damaged tissue, the body’s existing stem cells are stimulated and released to accelerate healing.
In PRP, the patient’s own blood is drawn and spun in a centrifuge to isolate the platelets and their associated growth factors. This concentration of cells is then added to the patient’s plasma which contains a variety of proteins that are essential to connective tissue healing.
Conditions responding well to this type of therapy include:
- Osteoarthritis of the joints
- Chondromalacia patella (patellofemoral syndrome/runner’s knee)
- Partial muscle tears, (hamstring strain)
- Meniscal (cartilage) tears in the knee
- Partial rotator cuff tears
- Persistent partial tendon tears and injuries, such as tennis elbow, plantar fasciitis, quadriceps, and patellar tendon tears.
Chronic Tendon Injuries
According to recent research, PRP is effective in the treatment of chronic tendon injuries, especially tennis elbow, a very common injury of the tendons on the outside of the elbow. The use of PRP for other chronic tendon injuries — such as chronic Achilles tendinitis or inflammation of the patellar tendon at the knee (jumper’s knee) is also promising.
Acute Ligament and Muscle Injuries
Much of the publicity PRP therapy has received has been about the treatment of acute sports injuries, such as ligament and muscle injuries. PRP has been used to treat professional athletes with common sports injuries like pulled hamstring muscles in the thigh and knee sprains.
Knee Arthritis
More and more literature is showing the effectiveness of low-leukocyte PRP in treating low- to moderate-grade knee osteoarthritis. Some studies have shown that these results can last up to two years.
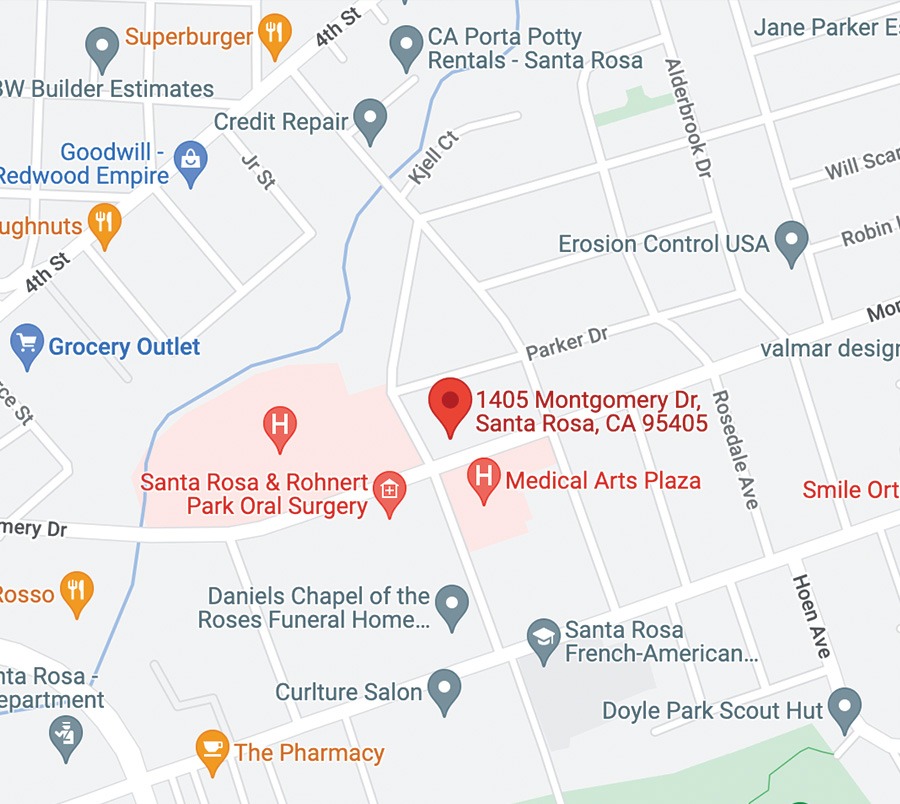
SRO Regenerative Medicine